Elephant in the Room – Astonishing Parkinson’s disease Beyond Tremors

The expression “Elephant in the room” is an metaphorical idiom used to describe something which everyone knows, but no one wants to mention or discuss it for various reasons. The above image is a part of “controversial art” by famous British artist Banksy. This art named “Elephant in the room” was featured as a part of US exhibition – “Barely legal” in 2006. It had it’s own set of controversies. However, the primary objective of this art was to highlight that billions of people lived below the poverty line. This art perse was a metaphor to speaking about elephant in the room and controversies there off.
Parkinson’s Disease is well known disorder where in people know issues about tremors, slowness, stiffness and walking related issues. However, there are many more other issues, which is well know to the patients, caregivers, and doctors, but most of the time, these symptoms are either brushed under the carpet or not enquired upon at consultation. Currently these features are becoming more important in the management of Parkinson’s Disease and more efforts are being put into the assessment and treatment of these issues. These are broadly classified under the category of Non Motor Symptoms (NMS) under the management of Parkinson’s Disease. However, these for all of us is the Elephant in the room which needs to be more outspoken and appropriate management needs to be done.
The International Parkinson Disease and Movement disorders society (IPMDS), has come up with exclusive scales on non motor symptoms to address this concern of elephant in the room.
“Elephant in the Room” – Parkinson’s Disease
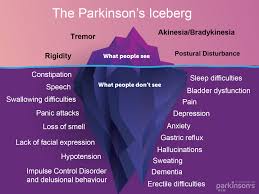
Image source: Parkinsonnsw
There are various symptoms which qualify for elephant in the room for Parkinson’s disease and prominent among them are
- Mood : All Parkinson’s disease patients might have some form of mood/behavioral changes, which is mostly under reported and only symptoms which become much bothersome are spoken about. Depression is one of the well know and needs to be tackled properly.
- Sleep : Sleep disturbances are common and sometimes predate the onset of motor symptoms by many years. These symptoms might include vivid dreams, nightmares, shouting/yelling/enacting in dreams (aka RBD), restless leg syndrome (RLS).
- Bladder issues : Urinary urgency, increased frequency, night time increased urinary frequency/volume are common bladder issues noted.
- Constipation : Constipation is probably one of well accepted and acknowledged symptom, which is noted well before the onset of motor symptoms
- Sexual dysfunction : Probably this is one of the least discussed non motor symptom, and mostly not addressed. The issue has to be discussed promptly by the patient or the doctor as its fairly treatable symptom
- Excessive sweating / drooling / skin oilyness : These changes are noted in patients with Parkinson’s disease and skin changes can be noted.
- Postural dizziness / fatigue : Patients with Parkinson’s disease tend to have
In the subsequent weeks, we will try to bring out exclusive write ups, including their symptoms, management, both on video and web write up. Effort will be put to get Kannada language audio/video files for the patients and care givers. Keep a lookout on the facebook page and youtube channel.