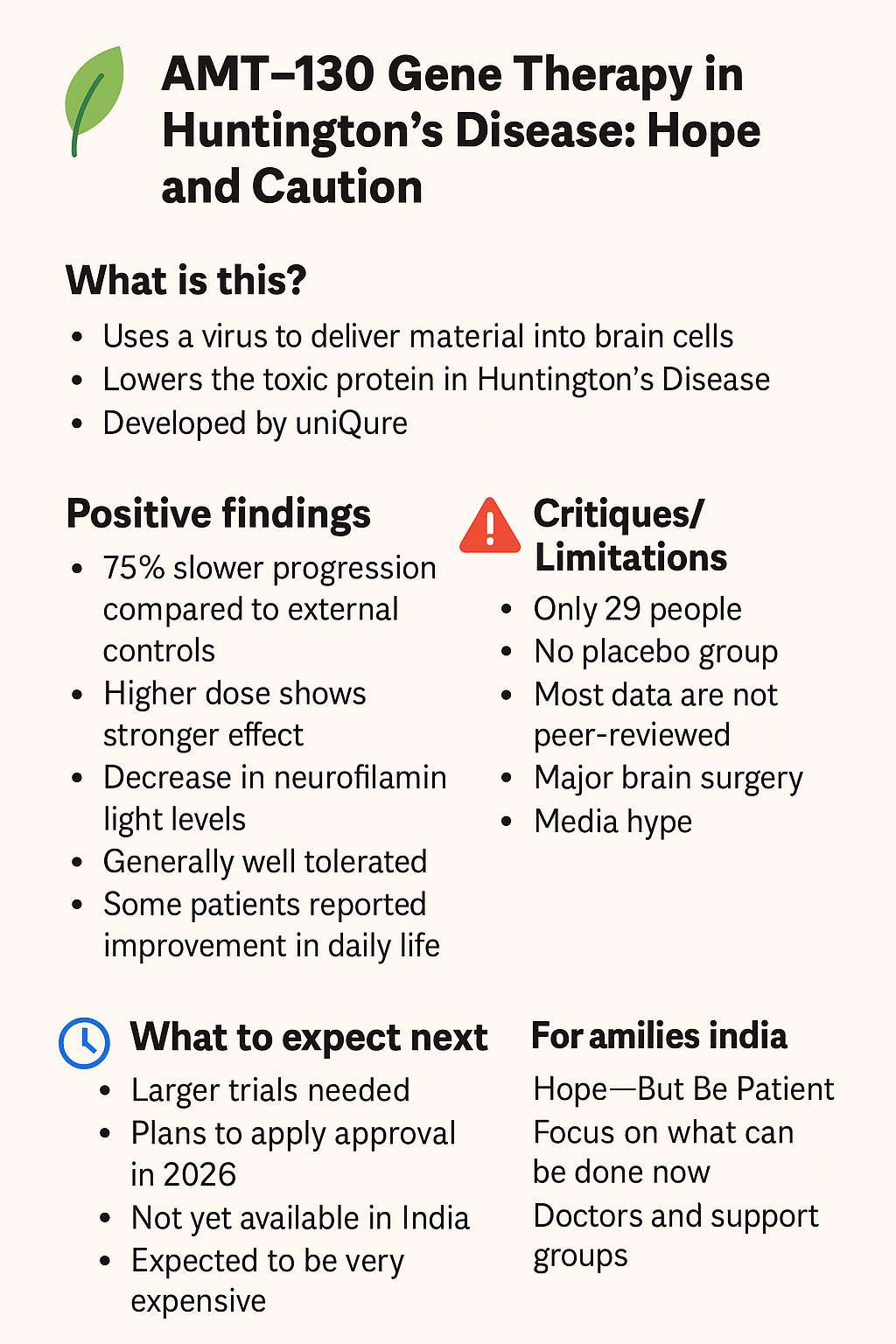
Huntington’s Disease in India: AMT-130 Gene Therapy Explained – Hope, Caution, and Costs
Introduction
Huntington’s disease (HD) is a rare, inherited brain disorder that affects thousands of families worldwide, including in India. It causes problems with movement, memory, and daily function, and currently has no cure.
In late 2025, news outlets and scientific groups around the world reported that a new experimental treatment — AMT-130 gene therapy — showed signs of slowing down the disease by up to 75% in a small clinical trial. Headlines have raised huge hopes. But what do these numbers mean? What are the positives, what are the limitations, and when could this treatment reach India?
This page explains AMT-130 in a Question & Answer format, using simple language for families.
Questions and Answers
1. What is AMT-130 gene therapy?
-
AMT-130 is the first gene therapy tested in humans with Huntington’s disease.
-
It was developed by uniQure, a biotech company based in the Netherlands and USA.
-
The goal: reduce the toxic huntingtin protein that damages brain cells in HD.
2. How does it work?
-
A harmless virus (called AAV5 vector) carries a small genetic code into brain cells.
-
This code produces micro-RNA, which acts like a “mute button” for the faulty huntingtin gene.
-
It stops brain cells from making as much toxic protein.
-
The therapy is given once, through 12–18 hours of neurosurgery, directly into brain areas called the caudate and putamen.
3. How was the study done?
-
29 patients with early Huntington’s disease joined the trial (low-dose and high-dose groups).
-
No placebo group was used. Instead, results were compared with historical/external controls (past patients with similar stage and age).
-
Patients are being followed for up to 36 months (3 years).
4. What are the positive findings?
✅ Slower decline:
-
At 36 months, decline on the cUHDRS scale was –0.38 points in treated patients vs –1.52 in controls → reported as 75% slower progression.
-
On another scale (TFC), decline was slowed by ~60%.
✅ Cognitive benefits:
-
~88% slower decline in processing speed (SDMT test).
-
~113% slower decline in Stroop word reading.
✅ Biomarkers:
-
CSF NfL (a marker of nerve injury) decreased by ~8.2% instead of increasing.
-
Early data suggested mutant huntingtin protein levels dropped by ~53.8% in some patients.
✅ Dose effect:
-
The higher dose group did better than the low dose group.
✅ Daily life impact:
-
Some patients reported better function — one returned to work, others were still walking when a wheelchair was expected.
✅ Safety:
-
Side effects (like inflammation and headaches) were manageable. No new major risks after 2022.
5. What are the critiques and limitations?
⚠️ Small trial: Only 29 patients, with just 12 in the high-dose group followed fully.
⚠️ No placebo group: Comparisons were against past data, not new untreated patients.
⚠️ Short-term issues: At 12 months, placebo/external controls looked better on some measures.
⚠️ Small effect size: On cUHDRS, the change (0.4 points in 3 years) may not be felt in daily life.
⚠️ Not peer-reviewed yet: Results mostly shared via company press releases and news.
⚠️ Surgery required: Long brain surgery with risks, so not a simple treatment.
⚠️ Cost and access: Gene therapies can cost over USD $2 million (~₹16–17 crore) per patient.
6. What does “75% slower progression” mean in real life?
-
It does not mean the disease is stopped or cured.
-
It means that, on paper, decline was slower than in comparison patients.
-
For example: what usually happens in 1 year might take 4 years.
-
This is encouraging, but based on small numbers and early data.
- Some of the experts have been critical of this 75% highlight and have discussed this on their social media handles. Quoting one of the experts interpretation on Twitter / X platform : “Primary outcome measure: the composite Unified Huntington’s Disease Rating Scale (cUHDRS). This is a measure of overall disability (0–25; lower = worse). Typical range: ~2–18. Results at 36 months: AMT-130 group: −0.38 Historical cohort: −1.52 The company called this a “75% slower progression.” Here’s how they got it: (−0.38 −(−1.52))/−1.52 × 100 = 75% · However, this 75% figure represents a relative difference compared to a propensity-matched historical cohort — not a within-patient change, nor a clinically meaningful effect on the cUHDRS scale itself. In short: it sounds big, but it isn’t) Here are the key caveats 👇 1️⃣ Small numbers: Only 12 participants completed treatment in the high-dose group (out of 17). Data for the low-dose group (n=12) weren’t reported. 2️⃣ Small effect size: The average decline in cUHDRS in early HD is ~0.9–1.0 points/year. A 0.4-point change over 3 years (0.13/year) is below the level patients can perceive as meaningful. 3️⃣ No concurrent placebo: The “75%” comparison is vs. a historical cohort, not a placebo group. Given the invasive protocol (brain infusion + repeated lumbar punctures), placebo effects could be substantial. 4️⃣ High variability, weak comparison: The cUHDRS has large standard deviations driven by practice and placebo effects. That variability can inflate small open-label trials when compared to natural history data.“
7. What happens next?
-
Regulatory steps: uniQure plans to apply to the US FDA in 2026. Europe and UK will follow.
-
Peer-reviewed publications are expected soon.
-
Larger trials with proper placebo groups are needed.
-
India: Availability will take several years. Access will depend on approvals, pricing, and neurosurgical facilities.
💰 Cost and Access Issues
-
Similar gene therapies (for haemophilia, spinal muscular atrophy) cost ₹16–20 crore per patient.
-
AMT-130 may be in this range or higher.
-
Because it requires specialised brain surgery, access will be limited to major centres even in high-income countries.
-
In India, widespread access will be a major challenge without strong public health or philanthropic support.
🌸 Final Words for Indian Families
AMT-130 is a milestone — the first time a gene therapy has shown signals of slowing Huntington’s disease. It brings hope but must be understood with caution:
-
Early trial, small numbers.
-
Headlines can exaggerate.
-
Costs will be very high.
For now, families in India should:
-
Stay updated through support groups and doctors.
-
Participate in registries and observational studies.
-
Hold on to hope — but avoid false promises.
📚 References and Further Reading
- https://x.com/AlbertoEspay/status/1976080543906398574