Understanding the Process of Deep Brain Stimulation (DBS) Surgery

When we decide or think to undergo Deep Brain Stimulation (DBS) surgery for Parkinson’s disease, the most common thought comes is HOW IS THE SURGERY DONE?. There are various steps before the surgery and you would have gone through these process like Levodopa challenge, cogntive assessment, decision making ability, speaking to people who have underwent surgery. BUT, still the question of how the surgery is done remains an intriguing enigma. In this blog we go through the process of SURGICAL DAY EVENTS along with the video and images to give an insight to all the people to understand the same. A brief visual overview of the events can be found on youtube : https://youtu.be/4QAugdLKYjg (This video link is available for above 18+ years only due to the descriptive videos)
One Day Prior to DBS Surgery
Most of the people planned for Deep Brain Stimulation (DBS) surgery are admitted a day prior to the surgery. Usually this day Patient and family gets settled after hospital admission process are finished. No medication changes are done on that day (If any changes are usually done atleast a week before – either stopping or adding). Surgical site preparation instructions are given by the surgeon (like head shaving / Part preparation etc). You would have your usual meal and medications before going to sleep.
On the Day of DBS Surgery
Your day begins around 6 to 7am in the morning, when the treating nurse checks and provides instructions. You would not be given any Parkinson’s disease medications (unless specifically indicated by the doctor) or food (you will be fasting overnight till the surgery is finished). You can take your other medications like for blood pressure etc. These would have been instructed to you a day before itself by the treating team and the Neuroanesthetist. Once your pre-surgical instructions are carried out by the nursing team (like part preparation, supervising medications), you would be shifted for the Frame fixation. From this point onwards your surgical day starts. We will go through them as step by step below.
Step-1 : Frame Fixation

You would be taken for Frame fixation, where in a box type frame is fixed on your head with local anesthesia. This box will act like a landmarks for various brain structures. (In simple way it like graph computation using X, Y and Z co-ordinates to locate different brain structure)
Step – 2 : Imaging of the Brain with Frame
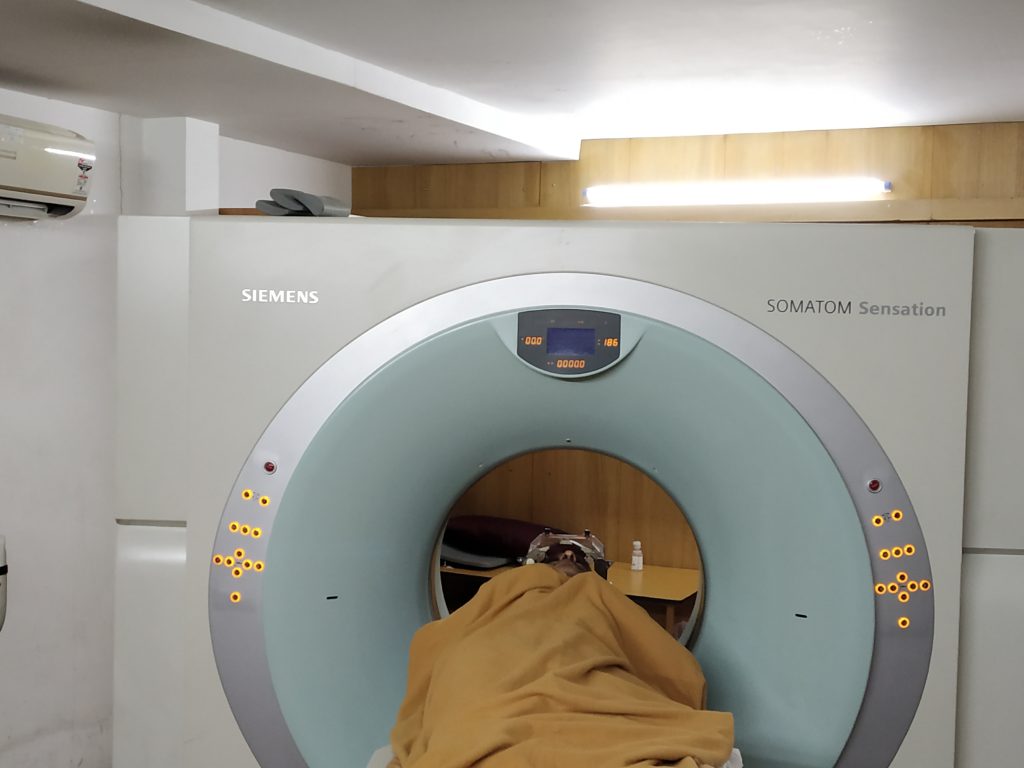
Following the fixation of the frame, you will undergo imaging (Commonly CT Brain is done. MRI can also be done). This will help to get the images of brain with the frame, which will act as anchor points to locate different distances in the brain.
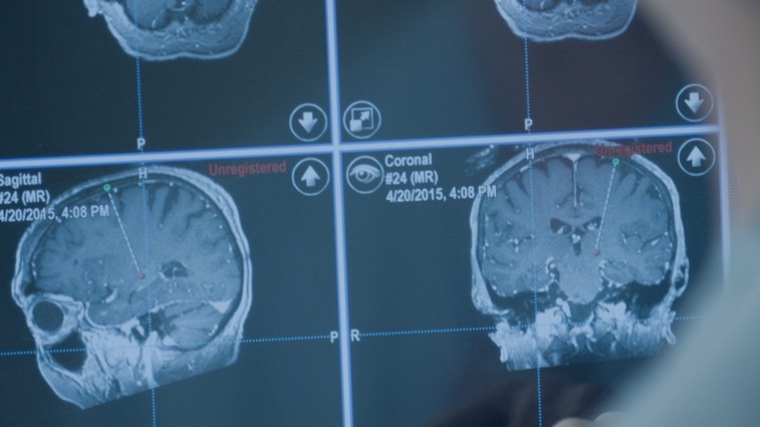
Step – 3 : Planning of the Surgical co-ordinates
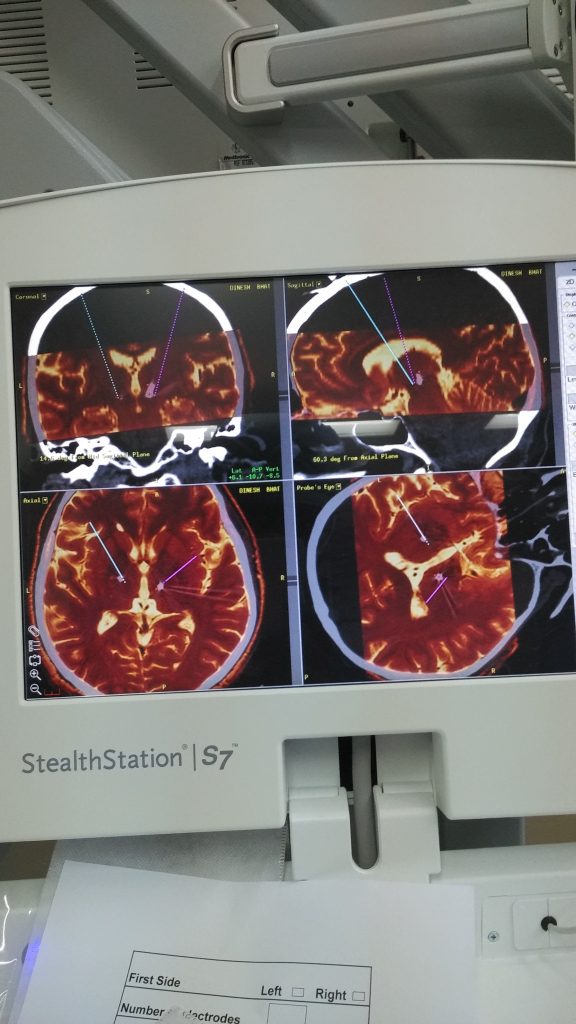
Once the imaging is done, you are shifted to the operating theatre room. Here you would be set in a comfortable position (so that you can stay like that for next few hours). In the mean time, the treating team will merge your images on a specialized software. From this software, they will choose the brain target (in PD mostly it would be subthalamic nucleus. Some time GPI is considered) and would be able to get co-ordinates based upon there distances from the frame anchor points. This will act as X, Y, Z co-ordinates of a 3d graph to target the brain.
Step – 4 : Positioning, Burr hole

Once the planning and co-ordinates for the surgery are finalized. The surgical team will set up a frame at the operating table. With this frame, then can mark the distances the electrodes to travel to reach the intended location. You would be awake or mildly sedated during this whole process. Once the frame is fixed a small hole is done in the skull (a size of a 25 paisa coin) to target one side of the brain. Later similar process with another hole is done to target other brain site. Once this is done, the scene is set up for assessment and target finalization.
Step – 5 : Microeletrode Recording
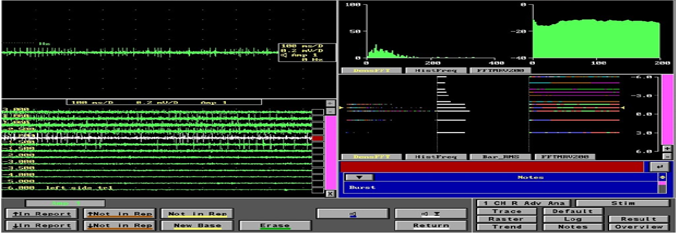
Once the burr hole is done a microdrive is fixed and fine recording electrodes are pushed in the planned trajectory. Each part of the brain has different electrical activity pattern and based upon which we can assume where the electrodes are going get placed. This is a method of re-affirmation of Imaging planning done previously and gives an confirmation of right position. Based upon these recordings the position of electorde is considered.
Step – 6 : Macro Stimulation and Clinical assessment

Once the microelectrode recordings are done, then the most important clinical assessment will start. In this step, small currents are given in the intended target region and clinical assessment for benefits would be done. This is point where patient has to be very alert and respond to various questions and tasks given by Dr. Prashanth LK. The benefits of stimulation and at voltages sides effects / excess effects are noted and recorded. This clinical assessment gives an final confirmation of the electrode placements.
Step – 7 : Electrode fixation
Following the electrode placement, it is fixed to the position and locked by a cap.
Step – 8 : Repeat procedure for the second site
After the electrode placement on one side, Step 4,5,6,7 are repeated on opposite side to fix the second electrode.
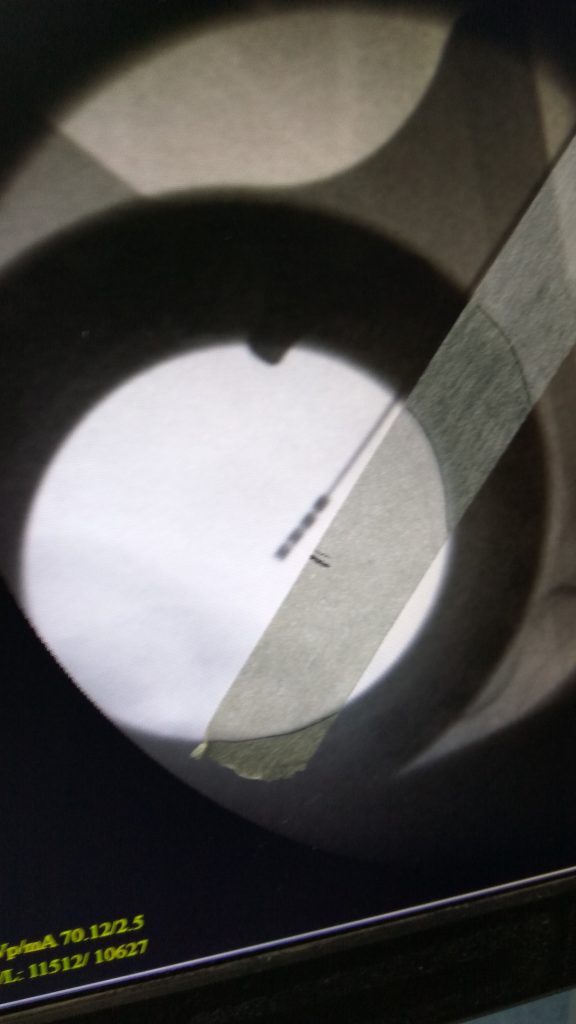
Step – 9 : Check Imaging
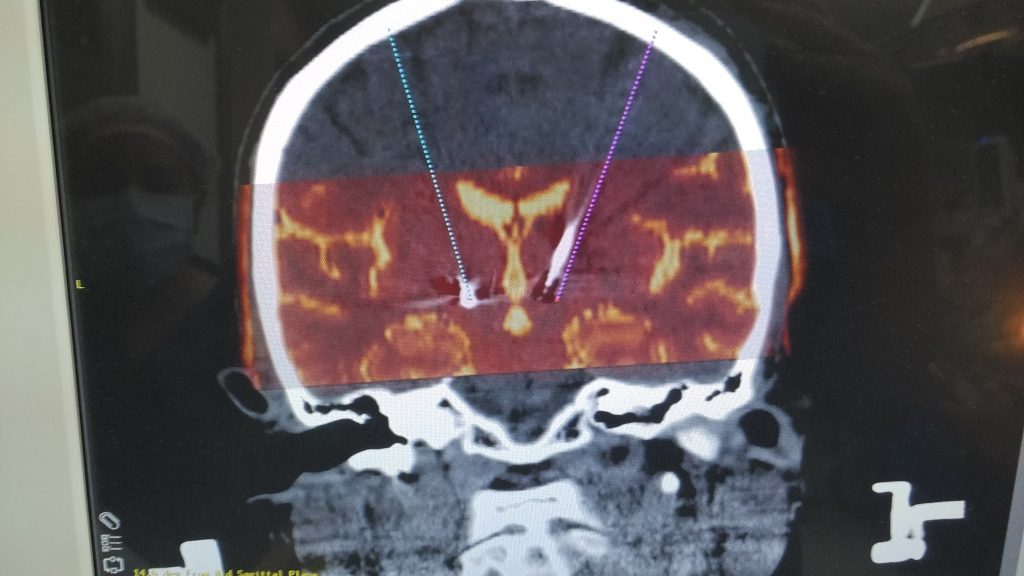
Once both the electrodes are fixed, a check imaging is done preferabbly and then these images are merged with the actual intended trajectories. The goal is to cross confirm the initial planned trajectories with the final fixed trajectories.
Step – 10 : Battery Placement
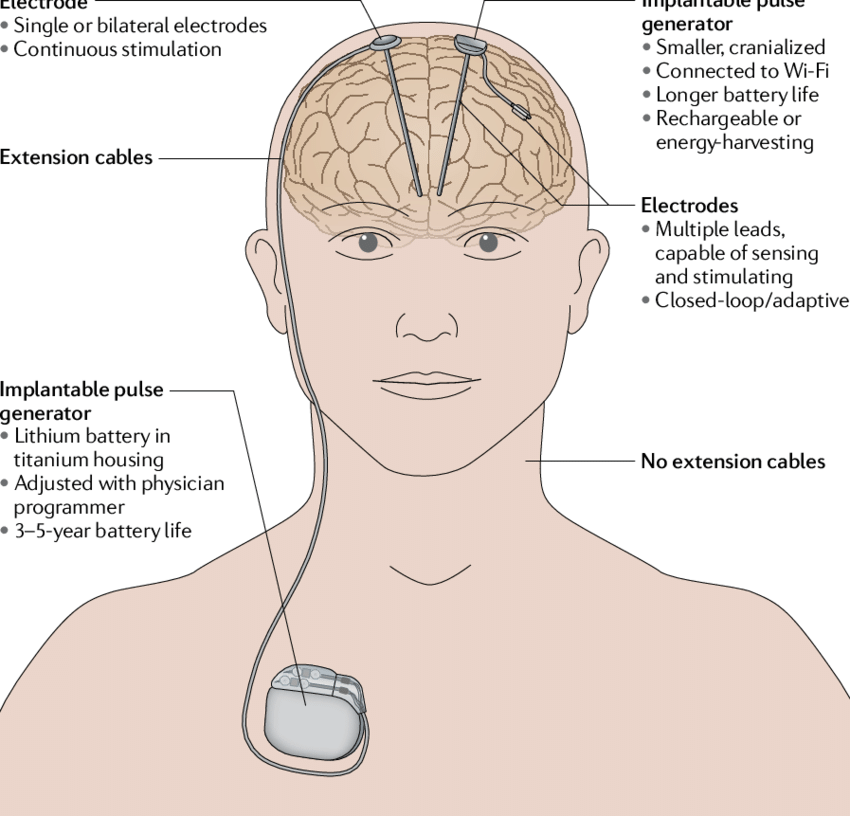
Following the check imaging, now you would be planned for battery placement. This point onwards you would be in general anaesthesia and deep sleep. A small pocket is made in your chest, just below the collar bone. After this an tunnel is created from the battery area to the head (Near the burr holes) just beneath the skin and both the parts are connected by the wire. Once all the electrical systems are connected, they are checked for integrity of the circuit, before closing the surgical sites. With this the surgical process is finished.
Step – 11 : Immediate Post Surgical care
Once the surgical process is finished you are weaned from the anesthesia and then shifted to the ICU. You would be awake (probably exahusted /sleepy). No oral feeds are given for another few hours at the discretion of the anesthesia team. Following that your regular Parkinson’s disease and other medications are started. You would be in the Intensive care unit overnight. There would some pain at the surgical wound points, but usually less as you would be given pain killer.
Step – 12 : Point to Remember
Please remember, surgical process is to fix the DBS stimulation system in the brain. The system is not yet assessed and started. It would be done subsequently at a later date. The whole surgical process lasts for 8-10 hours. In some patients the process may be staggered on different days, based upon the comfort levels of the patient and the surgical teams. There would be some deviations based upon each case to case basis, which would be discussed with the patient and family before and during the procedure (if required)
Day After the DBS Surgery
The next day following the Deep Brain Stimulation (DBS) surgery, you would be assessed. Most of the people would be back to normal status, with possible some sense of improvements, due to microlesional benefits. If you are deemed fit, then you would shifted to the ward, where you would stay for next few days.
Your whole stay in the hospital will last between 5-7 days on average.
Post Discharge
Post discharge, you would be guided on dates for surgical suture removals and planning for DBS programming.
The whole write up can be viewed as short 3 minute video on Youtube https://youtu.be/4QAugdLKYjg